📗 -> 05/29/25: NPB173-L16
🎤 Vocab
❗ Unit and Larger Context
Lecture 18: learning objectives
- Diathesis-stress model of depression.
- Major classes of antidepressant drugs.
- Serotonin neurotransmission.
- Monoamine neurotransmitters.
- Monoamine hypothesis of depression.
- Effects of ketamine on depression.
- Electroconvulsive therapy.
- Symptom clusters of schizophrenia.
- Typical antipsychotics.
- Atypical antipsychotics.
- Beyond the brain as a “bag of chemicals”.
✒️ -> Scratch Notes
Major Depressive Disorder (Depression)
Missed first two slides
Timeline of Antidepressants:
- Monoamine oxidase inhibitors (MAOIs)
- Tricyclic Antidepressants (TCAs)
- Teracyclic & Unicyclic Antidepressants
- Seratonin Antagonist & Reuptake Inhibitors (SARIs)
- Selective Seratonin Reuptake Inhibitors (SSRIs)
- Seratonin Norepinephrine Reuptake Inhibitors (SNRIs)
All traditional antidepressants have effects on serotonin (5-HT, because it’s chemical name is 5-hydroxytryptamine), a modulatory NT. Some have effects on other neurotransmitters as well.
Serotonin Neurotransmission
Serotonin is synthesized from the amino acid tryptophan
- This is the rate limiting step, tryptophan->serotonin
- No intermediate like LDOPA for serotonin
5-HT is loaded presynaptically into vesicles by VMAT2 transmporter
5-HT is cleared from the synaptic cleft by the serotonin transporter (SERT) (SER=Seratonin, T=transporter)into both glial cells and presynaptic neurons that use serotonin - block the transporter less serotonin would be released
Serotonin that undergoes reuptake by the releasing neuron can be reloaded into vesicles or broken down by monoamine oxidase (MAO) - block MAO 5-HT would be present longer
Monoamines as Neurotransmitters
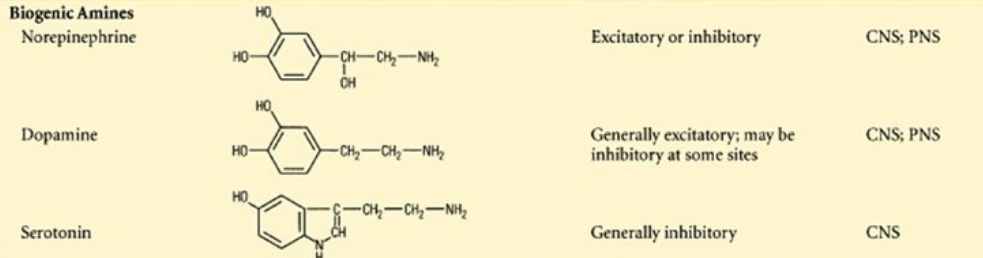
- Seratonin belongs to a larger class of neurotransmitters called monoamines based ontheir chemical structure. This class also includes dopamine and norepinephrine
- The similarity in chemical structure also implies some degree of similarity of interactions with other molecules, including receptors, transporters, and degrading enzymes. The amount of similarity can vary depending on the nature of the interaction.
- MAO inhibitors are antidepressants that limit the action of MAOs, enzymes that break down monoamines. MAO-A breaks down all three monoamines listed above. MAO-B preferentially breaks down dopamine.
- A major way to target increasing serotonin
- MAO-B isn’t ONLY dopamine, but is preferential for it
- Serotonin-norepinephrine reuptake inhibitors (SNRIs) reduce reuptake of both of these monoamines.
- Selective serotonin reuptake inhibitors (SSRIs) reduce reuptake of serotonin without effects on other monoamines.
- A major challenge in developing antidepressants is avoiding side effects.
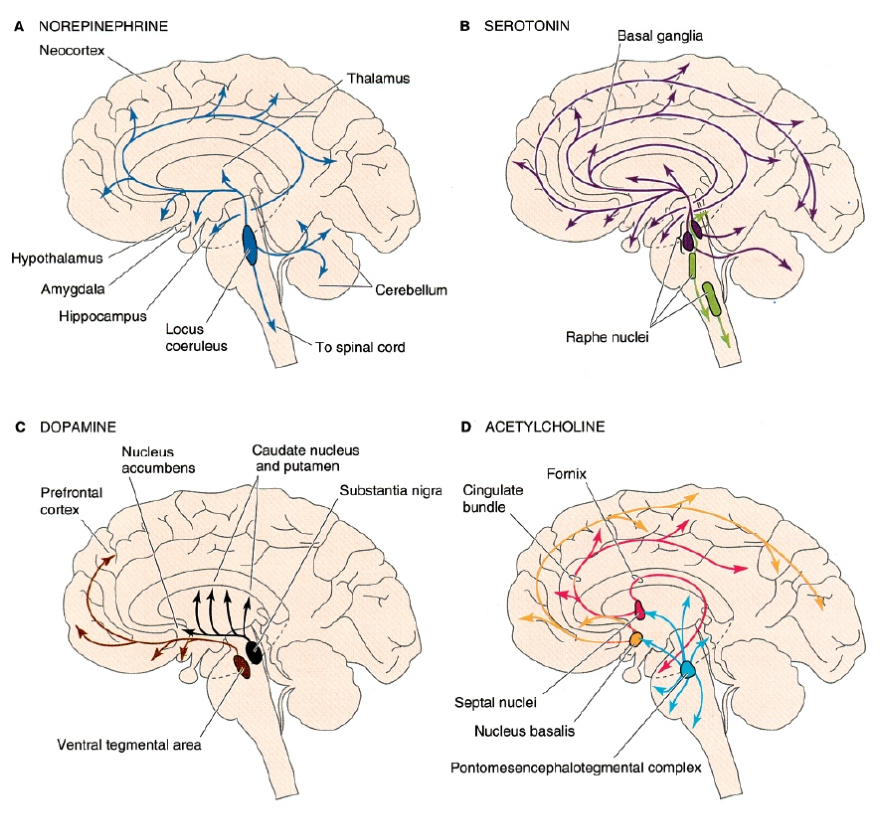
- Serotonin is primarily a neuromodulator in the CNS
- Neurons in the serotonin neuromodulatory systems have cell bodies in the raphe nuclei within the brainstem
- Almost every brain region receives input from serotonin neurons
- 7 different receptors for serotonin, with a range of possible effects
- Well known effects on mood, sleep, memory processing, and cognition
- Serotonin neuromodulatory system works in concert with other neuromodulatory systems, especially the other monoamines
Monoamine hypothesis Of Depression
- Monoamine receptors have large overlap in the signaling cascades that they influence
- The effectiveness of antidepressants has lead to the monoamine hypothesis of depression, that depression is caused by deficits in monoamine signaling
- However there is limited evidence of dysfunction of monoamine signaling that can explain depression
- Monoamines often have complex effects and interactions.
- For instance, lack of serotonin inhibits response reduction when pairing shock with previously rewarded behavior.
- Animals conditioned to pull a lever are less likely to if lesioned
- Additionally, their habits are not overcome by using an aversive stimulus (a shock). Their behavior is still at a relatively high rate, especially compared to the reduction of behavior in controls.
- As another example, serotonin reduces dopamine-induced increases in locomotor activity
- For instance, lack of serotonin inhibits response reduction when pairing shock with previously rewarded behavior.
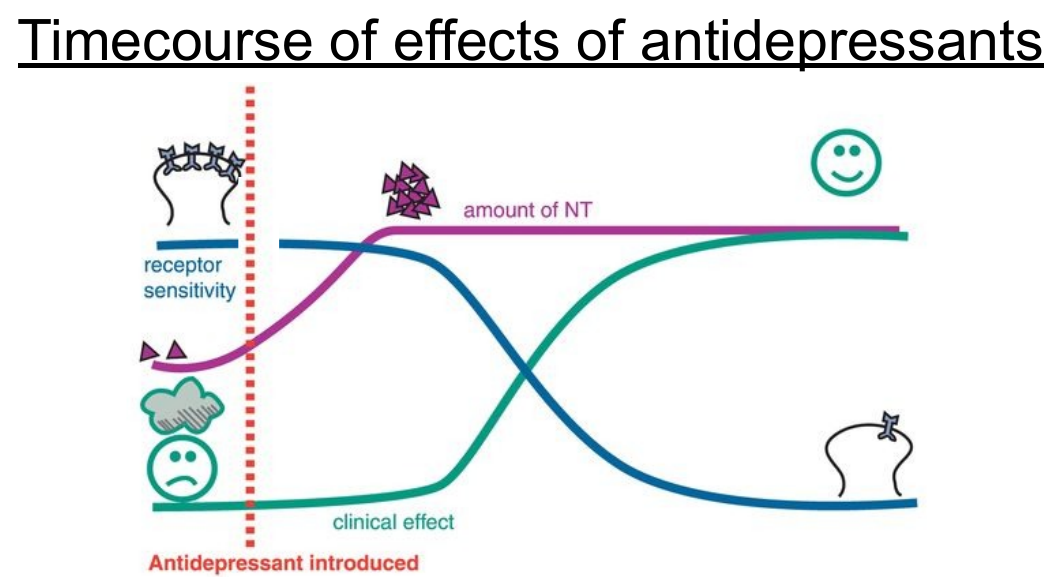
- Effects of antidepressants on neurotransmitter levels are fast (minutes to hours), but clinical improvement is much slower (weeks).
- This mismatch suggests that NT level itself is not the root cause of deficit
- More likely that altered NT lead to slower modifications involving neural plasticity that are more directly related to improvement
- As one example, sensitivity of receptors to monoamine neurotransmitters changes more slowly in response to the increase in NT levels
Ketamine
Ketamine (in low doses) can have fast effects on symptoms of depressions.
- In high doses, can be used for general anesthesia (and it is in animals)
Ketamine is an inhibitor of NMDA receptors for glutamate. Very distinct from pharmacological effects compared to classic antidepressants. - NMDA receptors play a critical role in synaptic plasticity, so ketamine’s efficacy for depression may involve immediate effects on mechanisms of synaptic plasticity, such as LTP
Electroconvulsive therapy for depression
- The last line treatment for severe depression that is not responsive to other treatments is electroconvulsive therapy. This is used only with informed consent and involves induction of small seizures through direct electrical stimulation of the brain.
- Patients are stabilized and monitored during the procedure. Treatment is usually given 2-3 times per week while symptom improvement is tracked.
- This procedure is effective for around 50% of individuals with major depressive disorder that was not improved by other treatments.
- The mechanism of action is unknown, but it does not relate in any established way to neuromodulatory systems.
Schizophrenia
A severely disabling mental disorder that affects how a person thinks, feels, and behaves.
- It has three clusters of symptoms: positive, negative, and cognitive
Schizophrenia has a high heritability (80%), higher than many psychiatric disorders
Schizophrenia usually starts in late adolescence and young adulthood - Sometimes described as a developmental disorder
Schizophrenia affects a greater percentage of males than females
Positive
Overt symptoms that should not be present.
Not ‘good’
Hallucinations
Delusions
Disorganized thoughts
Negative
Lack of characteristics that should be present
Reduced speech, even when encourages to interact (alogia)
Lack of emotional and facial expression (affective flattening)
Diminished ability to begin and sustain activities (avolition)
Decreased ability to find pleasure in everyday (anhedonia)
Social withdrawal (asociality)
Cognitive Deficits
Difficulties with following aspects of cognition can make it hard to live a normal life or earn a living
Memory
Attention
Planning
Decision Making
Typical Antipsychotics
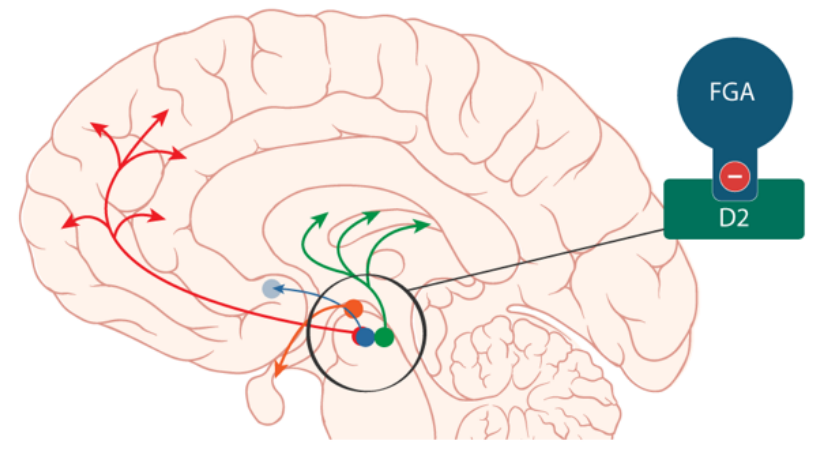
- Medications provide the first-line treatment for schizophrenia. Typical antipsychotic medications were first developed in the 1950s. Haloperidol (Haldol) and Fluphenazine (Prolixin) are examples.
- Typical antipsychotics have their primary effect via inhibition of D2 receptors in the dopamine system.
- There are four major dopamine pathways: the mesolimbic pathway from VTA to the nucleus accumbens, the mesocortical pathway from VTA to prefrontal cortex, the nigrostriatal pathway from SNc to the striatum, and the tuberoinfundibular pathway from the hypothalamus to the pituitary gland.
Effects of Typical Antipsychotics
Typical antipsychotics reduce the positive symptoms of schizophrenia, but no improvement in negative symptoms or cognitive deficits
Typically have numerous side effects:
- Dry mouth, weight gain, and movement disorders collectively called (extrapyramidal symptoms, EPS)
- Extrapyramidal symptoms involve dysregulation of the movement control circuits involving the basal ganglia through inhibition of D2 receptors.
Atypical Antipsychotics
- Pharmacological medications can be characterized by their binding affinity profiles, the set of receptors that they influence (and how).
- Typical antipsychotics have preferential (antagonistic) binding of D2 receptors.
- Atypical antipsychotics (or second-generation antipsychotics) have more complex binding affinities. This generally includes inhibition of 5-HT2A serotonin receptors.
- 5-HT2A is a specific type of serotonin receptors, one of the 5 mentioned above
- 5-HT2A receptors have wide-ranging effects, including inhibition of dopamine neurons. Thus, atypical antipsychotics allow more dopamine release while inhibiting D2 receptors.
- In some cases, atypical antipsychotics can be just as or more effective than typical antipsychotics with fewer side effects.
🧪 -> Refresh the Info
Did you generally find the overall content understandable or compelling or relevant or not, and why, or which aspects of the reading were most novel or challenging for you and which aspects were most familiar or straightforward?)
Did a specific aspect of the reading raise questions for you or relate to other ideas and findings you’ve encountered, or are there other related issues you wish had been covered?)
🔗 -> Links
Resources
- Put useful links here
Connections
- Link all related words