📗 -> 06/03/25: NPB173-L17
🎤 Vocab
❗ Unit and Larger Context
Announcements:
- Exam 3
- Final lecture
✒️ -> Scratch Notes
Lecture 14: Fragile X Syndrom
- Neurological vs. psychiatric disorders.
- Know the distinction between the two
- More about clinical approach in clinical approach in training, rather than fundamental distinctions
- Neuro: More salient signs of disorders. Objective 3rd person measurable characteristics
- Psych: Less salient signs. Often salient signs in what’s happening in mental functions
- Neuro and salient signs make treatment easier, know what has gone awry. More difficult for psych.
- Blueprint for treatment? review
- Neurodevelopmental disorders.
- Not mutual exclusive with psychiatric disorder
- Typically manifest during period of neurodevelopment / childhood / adolescence
- Fragile X
- Autism
- Schizophrenia arguably?
- Things not neurodevelopmental in nature:
- Depression / anxiety
- Fluctuates during lifetime
- Depression / anxiety
- Cognitive development and associated neural plasticity.
- Why so many neurodevelopmental disorders?
- So much change in development, so many coordinated things that must occur between/within brain regions
- So complex, many opportunities for things to go wrong
- Think about how plasticity can cause this review
- X-linked inheritance and X-chromosome inactivation.
- Know about X linked inheritance, and how this relates with chromosomes (parents, mom vs dad, carrier, etc.)
- Fathers with fragile X do not pass it on, nor do they have daughters
- Not just about genome, but also epigenetic. What environmental factors lead to chromosome activation / inactivation
- Depending on activation, depends on impact of mutation, correlates with damage/impact of fragile X
- Males will have it to the full severity, females will have graded impact depending on activation
- Could have 5% activation, but if its brain it will be highly manifested
- Know about X linked inheritance, and how this relates with chromosomes (parents, mom vs dad, carrier, etc.)
- Epigenetic regulation.
- Changes not in genome, but still affect protein expression
- Heritable, across cell division?
- May involved methylation of DNA, histone modifications
- Packaging of DNA affecting level of transcription of DNA
- Fragile X syndrome genetics and inheritance.
- Mutation on FMR1 gene on X chromosome
- A codon repeat mutation (CGG repeat in untranslated region, does not result in amino acid)
- Does not impact protein, impacts transcription
- <45 -> Normal gene
-
200 -> Full mutation
- 45-200 ->FX-TAS, not covered in class but intermediate
- Greater number of repeats affects transcription levels of protein coded for by FMR1 gene, the FMRP protein
- Leads to tighter packaging of gene, reduced transcription, reduced protein
- Fragile X syndrome epigenetics.
- About something that involves transcription, not the protein itself
- Not explicitly the same as other epigenetics, but shares the fact that it is not directly a change in genome, but changes in expression (similar to other epigenetics)
- FMRP: regulator of protein expression and synaptic plasticity.
- Fragile X does not affect FMRP (protein coded) structure/function, but affects its expression
- FMRP regulates other proteins.
- Stalls protein translation of those involved in synaptic plasticity
Graph Slide
- Cognitive capacity peaks in young adulthood, then gradually declines in later adulthood
- In normal decline, called senescence
- Total number of synapses across a lifetime
- In dramatic change of neural development (cognitive capacity), there are also enormous changes at the level of synapses and synaptic plasticity. After their peak in the critical period, they stabilize in total number. Plasticity continues.
- Critical periods are allowed by increases in synapse number during their respective critical period. Not necessarily neuron number, but synapse number
- Early critical periods in seeing/hearing (peak at 4 month)
- Intermediate critical period in language/speech (9 months)
- Later critical period in higher cognitive functions (4 years)
Neurotransmitter slide
FMRP - Protein for fragile X syndrome
Presynaptic terminal
- In healthy/diseased, both will release neurotransmitter (glutamate)
- Glutamate can bind to multiple different receptors
- AMPA receptors are the fastest glutamate receptor, ionotropic receptors. Will open and be permeable to sodium leading to quick depolarization (level of ms)
- NMDA receptors also bound by glutamate receptors. However, they are blocked by magnesium. The magnesium block is released when cell is depolarized, and allows ions to pass through, including calcium. (leads to post synaptic events)
- Leads to slower depolarization that AMPA
- mGluR5 - Metabatropic Glutamate Receptor 5.
- One of its effects is to promote proteins that are usually blocked by FMRP.
- Push pull regulation between mGluR5 and FMRP
- When proteins get through, they remove AMPA receptor
- If we have enough glutamate to highly excite the synapse, maybe we can make it less sensitive by removing AMPA receptors
- Backwards, we can strengthen synapse by inserting AMPA receptors.
Postsynaptic terminal
- In healthy, FMRP helps to downregulate protein synthesis in post synaptic cell
- In diseased, FMRP is less expressed, and won’t be able to downregulate as much. Proteins will be overproduced, and AMPA receptors will be removed.
Lecture 15: Autism
No known genetic cause, but it is comorbid with Fragile X (fragile X sufferers more likely to get Autism)
-
Fragile X one of the largest known genetic causes of autism (still relatively lol)
-
The DSM as a guide for classification of mental disorders.
- Provides criteria for diagnosis
- Not set in stone, evolve over time and many revisions/iterations
- Not full consensus, but provides useful guidelines
- Provides criteria for diagnosis
-
The triad of autism symptoms.
- Autism spectrum disorders now
- Recgonize the triad of symptoms. Core elements of autism disorders:
- Difficulties with social development
- Difficulties with communication
- Difficulties with repetitive behaviors
-
Autism as a spectrum disorder.
- No clear dividing line between typical/divergent. A spectrum/gradation levels of severity
- Multiple dimensions involved too, independent/semi-independent symptom categories
- Severe symptoms with repetitive behaviors, but less severe for communication e.g.
-
Autism diagnosis and increasing prevalence.
- One of the most salient things about autism/adhd is the increasing prevalance. Far more common now
- A major factor is the change in diagnosis criteria
- Debate in whether something now is actually causing increased spread
- Could be seen as bad, or good in helping to better understand the diseases
- One of the most salient things about autism/adhd is the increasing prevalance. Far more common now
-
Assessing genetic contributions to mental disorders.
- GWAS - Genome Wide Assocciation Studies (can find correlations in genetics)
- Or quantify genetic vs environmental studies
- Twin studies: Compare individuals who are identical twins vs those who are not. Then find the congruence/correspondence of the development of a disorder in identical/non-identical twins.
- Highest level of correlation/correspondence/congruence: all sets of twins, they have equal development of disorder (not/not or have/have)
- Should only expect a reduction in identical/non-identical correspondence if there is a genetic role.
- Heritability: Number between 0 and 1. Proportion of variability explained by genetics rather than environment.
- Genetics > Environment: High heritability
- Environment > Genetics: Low heritability
- Twin studies: Compare individuals who are identical twins vs those who are not. Then find the congruence/correspondence of the development of a disorder in identical/non-identical twins.
-
Absence of any link between vaccinations and autism.
- Absolutely sure there is no link. Highest power statistic result in modern biology?
-
Social development in autism.
- Autism we better understand mechanisms/changes that could create these symptoms (at least compared to fragile X)
- Face recognition different. Some studies suggest changes in FFA, and processing of faces with autism
-
Theory of mind.
- Ascribe distinct beliefs to one other than oneself (Saly Ann test, the box hypothetical, one person not knowing that the toy was moved from box a to box b, where do they look for toy first?)
- Recognize when theory of mind works properly vs not
-
Language development in autism.
- Know a decent amount about neural mechanisms
- Wernicke’s / Broca’s
- Complexity of interpretation of stimuli. Basics of perception all the way to ascribing meaning to sounds. Possible hints to look into for pathophysiology.
- No clear smoking guns yet.
-
Brain changes with autism.
- Biggest observation, accelerated/overgrowth of neural development early on, then slower growth later on. Brain size reaches similar size by end.
- Not thought to be full cause, but another sign to look into.
- Biggest observation, accelerated/overgrowth of neural development early on, then slower growth later on. Brain size reaches similar size by end.
-
Critical periods in neurodevelopment.
- During critical period in increase in number of synapses, increased capacity for learning.
- Afterwards, prune/whittle down the capacities of learning with experience/learning
- You NEED to have experience during these critical periods in order to develop correctly and take advantage of the critical periods
- During critical period in increase in number of synapses, increased capacity for learning.
Graph Slides
- 3 different categories
- Social
- Behavior
- Communication and language
- Autism is a spectrum
- Brain size/growth. Overgrowth early, arrested growth later.
Think about connecting the growth to different categories in autism.
- Repetitive behavior links with decision making?
- Brain structures involved in that
Lecture 16: Attention Deficit Hyperactivity Disorder
- ADHD signs and symptoms.
- Pneumonic: For autism, adhd and schizophrenia they each have their own triad.
- ADHD triad:
- Attention/Distractability. Difficulty in sustaining attention for long periods of time in a context dependent manner
- Hyperactivity. In the name too. Increased levels of activity, movement or speech. WANTING to act/move, acting as a distractor.
- Impulsivity. Contrasted with deliberation. Make decision quickly, with less accumulation of evidence. Not a bad thing necessarily, but overshooting the balance
- Function magnetic resonance imaging.
- How can we measure human cognitive faculties?
- Take clinical measurements possibility
- Can take non-invasive measurements with fMRI
- Proxy of activity, BOLD response (Blood Oxygenation Level Dependent signal)
- Bad in the sense:
- it doesn’t measure individual neurons
- could even have multiple activities cancel each other out, not be noticed
- Slow, metabolic
- Default mode network and ADHD.
- Default mode network: Particularly active when not paying attention to external world. Daydreaming internally
- Is this related to distractability in ADHD?
- DMN pulls attentional capacities from attention engaged networks?
- Default mode network: Particularly active when not paying attention to external world. Daydreaming internally
- Neural mechanisms of attentional allocation
- Other networks involved too: ?
- Basic idea of attention allocation, areas of brain involved in sensory processing are more active when are paying attention
- Then, they have greater impact on other processing in the brain, potentially on decisionmaking. This is how we can get benefits from paying ‘attention’
- Neural mechanisms of impulsivity.
- Neurons that seem to accumulate decisions over time to reach a decision
- Simple as hitting snooze button vs waking up e.g.
- Might be a long decision, take a long time (deliberative, factor in internal evidence, like what you have to do)
- Or be impulsive, and just snooze without thinking
- A more impulsive decision is less evidence accumulated over time
- Lower threshold needed?
- Neurons boosted externally?
- Stimulant-based treatment of ADHD.
-
5% of school age children prescribed medication for ADHD
- They are effective, but unclear why. They impact dopamine neurotransmission
- Ritalin and Adderall block dopamine transporter (dopamine sits in cleft for longer period of time)
-
- The role of dopamine in ADHD.
- Effectiveness of Ritalin and Adderall suggest that dopamine plays a role somehow
- However, not necessarily causal. For example, there could be some other problem in the striatum, and it can just be mitigated by upping dopamine signaling in the striatum.
- Not necessarily dopamine the root cause, but it can be addressed/medicated with the dopamine transporter inhibitor. Important distinction
- Neurotypical vs. neurodivergent.
- Individuals with ADHD/Autism frequently identify distinctions in their experiences with those who do not
- Maybe not a disorder/disease, but potentially a condition
- Destigmatize things that are psychiatric
- Lots of treatments discovered, lots of people who don’t have access to it or don’t seek it / avoid it
Graph Slides
Default Mode Network: Not needed to memorize, but blurting them down:
- PCC - Posterior Cingulate Cortex
- RSC - Retrosplenial Cortex
- PHC - Parahippocampal Cortex
- HF - Hippocampal Formation
- vmPFC - ventromedial PFC
- amPFC - anteromedial PFC
- dmPFC - dorsomedial PFC
- IFG - Inferior Frontal Gyrus
- TPC - Temporoparietal Cortex (often refers to TPJ: temporparietal junction)
- LTC - Lateral Temporal Cortex
- IPL - Inferior Parietal Lobule
- pIPL - posterior Inferior Parietal Lobule (overlap with angular gyrus?)
- Medial temporal subsystem: HF, PHC, RSC
- Core hub: PCC, aMPFC, vmPFC
- Dorsomedial subsystem: dmPFC, IFG, IPL, LTC, TP
Spatially distinct location, distributed
Tend not to involve early sensory/motor areas. Instead, association cortex areas.
- More involved in internal/thoughtful processing
- Not so much involved with immediate control
Changes in activity levels across brain networks:
- DMN in pinkish/purple
Main take home message is that all individuals have activity in DMN and other more attentive networks, but fractions of activity in each network has been established as differing (at least probabilistically) among control patients and ADHD - Could be helpful in tracking down neural substrates?
Lecture 17: Anxiety Disorders
- Anxiety vs. fear.
- Not clear cut, but:
- Fear: Response to immediate/perceived to be immediate danger
- Anxiety: Similar response in the anticipation to some future danger.
- Adaptive or maladaptive
- Evolutionary holdover present in many species, largely maladaptive to modern contexts
- Not clear cut, but:
- Types of anxiety disorder.
- Clearly:
- Generalized Anxiety Disorder (GAD)
- Phobia / Social Phobias / Specific Phobias
- Also potentially classified:
- PTSD
- OCD
- Not mentioned but also:
- Panic disorder
- Clearly:
- Memory networks in the brain.
- Cerebral Cortex - Long term declarative memories
- Striatum and Cerebellum - Procedural memory
- Hippocampus - Critical for memory formation
- PFC - Working memory, holding onto things short term
- Amygdala - Emotional Memory
- Role of the amygdala in fear and anxiety.
- Amygdala - Controller over fear and anxiety responses.
- Also holds memory for things/processes/external stimuli that should induce fear & anxiety responses
- Probaby not just amygdala, but amygdala well established as being a central player with these responses
- Amygdala - Controller over fear and anxiety responses.
- Hippocampal role in memory consolidation.
- Don’t need it for HAVING long term memories, needed to consolidate them however
- Hippocampal role in representing space and environmental context.
- Why is HPC needed for memory consolidation?
- It provides information about environmental context
- Place cells, literal space context
- Pattern of activity not one neuron
- Crucial for forming memories, and crucial for accessing memories
- Sometimes plays role beyond forming memories
- It provides information about environmental context
- Why is HPC needed for memory consolidation?
- Associative learning.
- Forming connections between 2 or more stimuli.
- Classical conditioning (pavlovian)
- Operant Conditioning (action with a stimulus)
- Hebb’s rule.
- The neural mechanisms behind associative learning
- “Neurons that fire together wire together”
- Long term potentiation (LTP).
- Allows for Hebb’s rule.
- NMDA?
- Provides constraints on Hebb’s rule. Not just any two neurons active together, an axon between helpful. Need to fire together AND have a capacity to change their synaptic strength. an axon growing close to a dendrite, and a dendritic spine causing there to be a connection
- The amygdala and hippocampus in fear conditioning.
- We can imagine them working together to encode a fear response
- Fear extinction.
- An active process to repeatedly present a stimulus with no (associated response?).
- Slowly extinguishes learned association
Graph Slide
Neural Mechanisms of Learning:
- A salivation neuron that triggers an action (salivation)
- A food detector neuron that responds when food is present (has strong connection with salivation neuron)
- A third neuron that responds strongly to bell. Initially very weak connection to salivation
- When the bell and food detector neuron are paired together, there will be a post synaptic activation of the salivation neuron, presynaptic activation of the bell neuron, and by Hebbs rule we have wiring together (LTP)
Grossly oversimplified but rough idea
Amydala regions:
- 3 main parts,
- Lateral (LA)
- Basolateral (BLA)
- Central (CeA)
- Input is processed from other brain regions (sensory cortex, PFC, HPC) in the LA
- In the processing there is a large amount of internal inhibition via ITC (intercolated) cells using GABA
- CeA is the primary part of the amygdala sending outputs to other bain regions
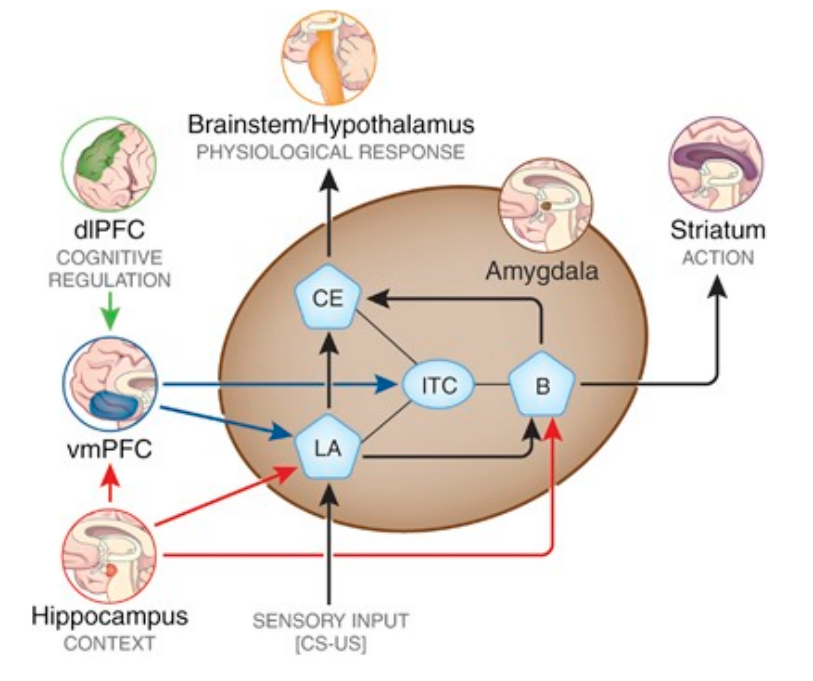
- LA (lateral) receives input
- Projects to CE (central) and B (basolateral).
- During this, a lot of ITC inhibition
- Needs to be overcome in order to create a response
- Environment potentially, shocks, pavlovian learned responses, context (HPC)
- During this, a lot of ITC inhibition
- CE induces a physiological response in Brainstem/Hypothalamus
- B induces a action with the striatum
BODY WIDE responses
Lecture 18: Depression and Schizophrenia
-
Diathesis-stress model of depression.
- Predispositions to depression (second hits/third hits?)
- Diathesis - Negative predisposition, vulnerability to being afflicted in combination with other factors
- Life circumstances
-
Major classes of antidepressant drugs.
- 3 Major ones to know
- MAO Inhibotors
- MAO is an enzyme that breaks down seratonin and other monoamines
- Inhibiting this leads to more monoamines
- SNRIs - seratonin norepinephrine reuptake inhibitors
- Blocks reuptake of the NTs
- SSRIs - selective seratonin reuptake inhibitors
- Blocks reupate of seratonin through selectively blocking the seratonin transporters (SERT)
- MAO Inhibotors
- These 3 major ones all lead to upregulation of seratonin
- 3 Major ones to know
-
Serotonin neurotransmission.
-
Monoamine neurotransmitters.
- Seratonin, norepinephrine, dopamine all monoamines.
- All work together, unclear how they interact to lead to impacts on depression
-
Monoamine hypothesis of depression.
- Strong version: Pathophysiology of depression is caused by some deficit in monoamine neurotransmission
- However, just having MAO inhibitors helping depression symptoms does NOT mean that this is true
- In fact, evidence against this with the timing of antidepressant effectiveness
- Very fast effects on neurotransmission (minutes/hours) , but clinical impacts slower (days/weeks/more)
- Also challenged by ketamine
- Strong version: Pathophysiology of depression is caused by some deficit in monoamine neurotransmission
-
Effects of ketamine on depression.
- Ketamine - an NMDA inhibitor
- No idea why it works
- Effective rather quickly for depression. This would suggest a perhaps ill informed NMDA hypothesis of depression
- We should consider instead that they are somehow altering brain states / or addressing symptoms
- NMDA receptors are critical, impacting them is a large shift
- Ketamine - an NMDA inhibitor
-
Electroconvulsive therapy.
- No idea why it works
- Changes brain states while applied, maybe that helps? Effective in 50% of patients (often antidepressant resistant depression)
-
Symptom clusters of schizophrenia.
- Positive symptoms: Fluctuate more, better addressed by meds.
- Negative cognitive: Often more impactful, because more difficult to treat
- Positive: Things that happen that we wouldn’t want to happen.
- Delusions / Hallucinations
- Antipsychotics effective in reducing thse
- Negative: Things absent that we would want
- Lack of: Motivation / Social Desire / Eating / Sleeping
- the above are usually absent or reduced
- Lack of: Motivation / Social Desire / Eating / Sleeping
- Cognitive: Mental faculties implacted
- Difficulties with memory / planning / cognitive capacity
-
Typical antipsychotics.
- All these work by inhibiting the D2 receptor (dopamine receptor in the indirect pathway in the striatum)
- Also a receptor in other pathways, in particular within frontal cortex
- Can have complex mechanisms, expressed on dopaminergic neurons themselves. An autoreceptor to itself?
- Why do they help? We dont know
- Pushing the brain state around, ends up helping
-
Atypical antipsychotics.
- Differ from the typical approach of inhibiting the D2 receptors
- Also inhibit 5-HT2A (a specific seratonin inhibitor)
- Hope to be effective similarly to typical meds, but overcoming/mitigating the side effects associate with typical meds
- Also tend to have more complex binding affinity profiles that typical antipsychotics
-
Beyond the brain as a “bag of chemicals”.
- Not about the balances of neurotransmitters, but about these being modulators we can use to push around brain states
- He encourages us to take a look at the brain state extra reading (described on the class home page)
Graph Slide
Know about life cycle of serotonin:
- Synthesis
- Tryptophan -> Serotonin
- Storage
- VMAT2 transports serotonin into vesicles
- Release
- Vesicle releases serotonin into synaptic cleft
- Activation
- Binds to receptors and initiates a signal to the cell body of post synaptic cell
- Clearing
- Receptor clears.
- Taken up by:
- Presynaptic neuron (SERT)
- Glial cell (SERT too?)
- Leaves the cleft through diffusion
- Reuptake
- After reuptake, serotonin gets reloaded into vesicle (->VMAT2) or broken down (->5-HIAA)
- Metabolism
- MAO breaks down serotonin
Appreciate different monoamines work through different receptors with different impacts, but they’re all related to each other
- Medication effective because we have different ‘knobs’ we can turn, and their resulting downstream impacts of adjusted neural state
Be familiar with binding affinity profiles
- Think about D2 and 5-HT2A with respect to schizophrenia
Think about brain as complex dynamical system
🧪 -> Refresh the Info
Did you generally find the overall content understandable or compelling or relevant or not, and why, or which aspects of the reading were most novel or challenging for you and which aspects were most familiar or straightforward?)
Did a specific aspect of the reading raise questions for you or relate to other ideas and findings you’ve encountered, or are there other related issues you wish had been covered?)
🔗 -> Links
Resources
- Put useful links here
Connections
- Link all related words